
"Serving Clinton, Essex, Franklin, Jefferson,
Lewis, St. Lawrence, Warren and Washington Counties"
Not all healthcare takes place in clinical settings like doctors’ offices, hospitals, or health centers. When a community member needs care as fast as possible, Emergency Medical Services (EMS) providers are the first to respond, providing critical care at the scene, in the back of an ambulance, or even aboard a rescue boat, helicopter, or other emergency vehicle.
Because of its role on the “front line” of healthcare, EMS operations require a great deal of planning to ensure consistency, quality, and seamless cooperation with local hospitals, 911 centers, and other agencies. In the North Country, FDRHPO assists with this planning and facilitation through its partnership with the EMS Program Agency.
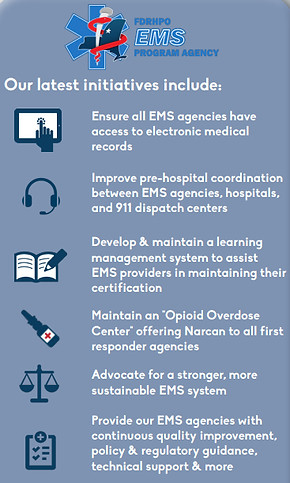
As one of 18 program agencies in New York State, the North Country EMS Program Agency oversees operations of more than 170 EMS organizations across Clinton, Essex, Franklin, Jefferson, Lewis, St. Lawrence, Warren, Washington, and parts of Hamilton counties — most of which are staffed by volunteers from their communities. For all of these EMS organizations, the Program Agency provides…
-
Continuous Quality Improvement
-
Policy and Regulatory Guidance
-
EMS Training and Credentialing
-
Technical Support
-
and more!
Through the guidance of the Regional Emergency Medical Services Council (REMSCO) and the Regional Emergency Medical Advisory Committee (REMAC), the Program Agency also works with educational institutions, 911 centers, hospital emergency departments, law enforcement officials, and other stakeholders to ensure the entire EMS system runs smoothly. These two regulatory bodies are composed of regional experts who meet quarterly to discuss current policies and procedures. To learn more about the North Country REMSCO and REMAC, click here, for Mountain Lakes REMSCO and REMAC, click here.
